PPN
This topic is intended for Rexall pharmacies only and is not applicable to Independent pharmacies.
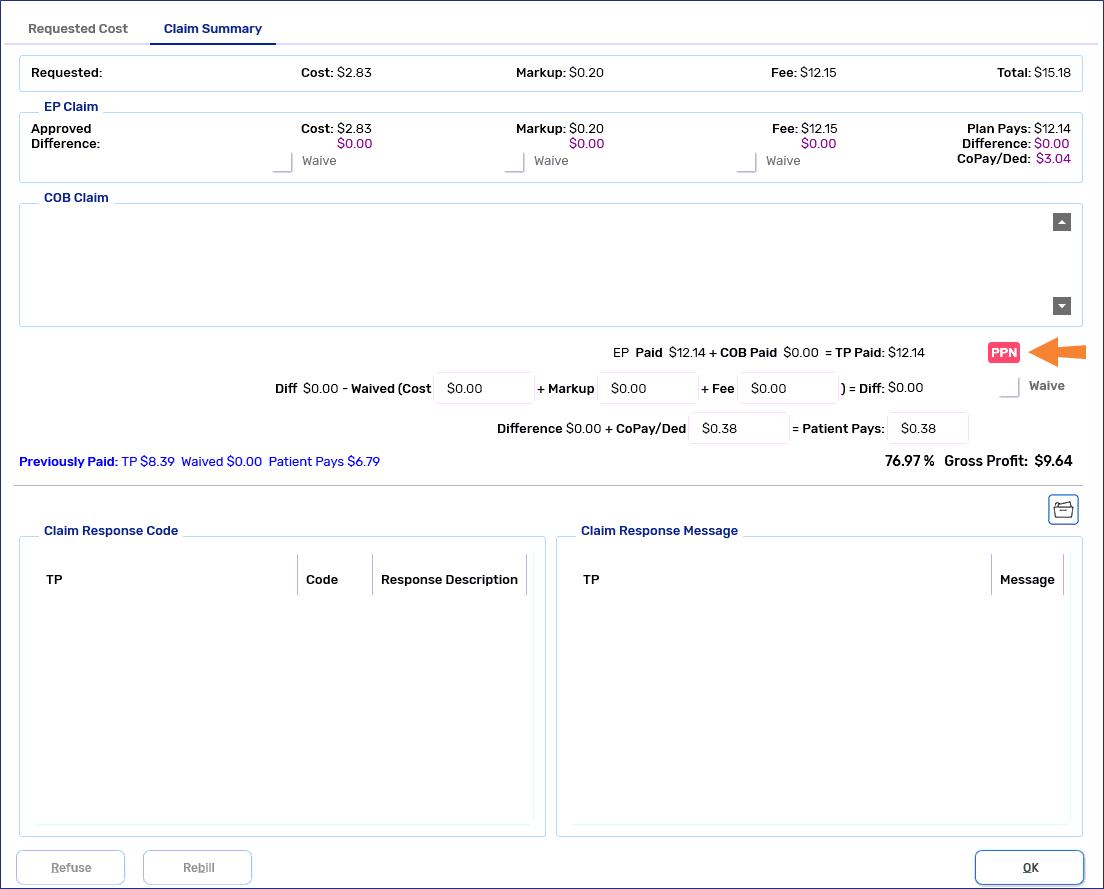
When Third Party plans are part of a Preferred Pharmacy Network (PPN), a PPN indicator ![]() will display in Propel Rx when prescriptions are adjudicated to these plans. If a primary Third Party payor added falls under PPN, you will see a PPN indicator in the following locations:
will display in Propel Rx when prescriptions are adjudicated to these plans. If a primary Third Party payor added falls under PPN, you will see a PPN indicator in the following locations:
-
Rx Detail Price section and Requested Cost window beside the Total field
-
Claim Summary window above the Waive checkbox in the middle
When changes are made to the prescription's QA, Qty, DS, Bill Codes, or Drug that changes its qualification under a PPN, the display of the indicator will be re-evaluated.
If the prescription's price (Cost, Markup, Fee) is changed after a PPN indicator is displayed then the indicator will remain unless a parameter is changed that triggers a re-evaluation.
PPN Waives
In some situations, automatic waive amounts are applied when prescriptions are adjudicated to Third Party plans that are part of a PPN. When there are multiple PPN Third Party plans that the prescription is billed to, the PPN Waives apply in the same order as the billing codes.
There are 3 types of PPN Waives that can be applied for a prescription. To learn more about each type of waive, use the dropdowns below.
A fixed dollar amount is waived from the CoPay/Deductible. When the dollar amount is greater than the CoPay/Deductible, the remaining amount of the waive will be applied to the sum of the cost, markup, and fee differences.
The difference between the submitted dispensing fee and the PPN negotiated fee is waived from the CoPay/Deductible. When the difference is greater than the CoPay/Deductible, the remaining amount of the waive will be applied to the sum of the cost, markup, and fee differences.
A percentage of the total approved cost, markup, and fee is waived from the CoPay/Deductible up to a maximum amount. A maximum waive amount will be applied to the individual cost, markup, and fee differences.